From Aches to Answers: Osteoarthritis FAQs
- Good Country Physio

- Aug 8, 2025
- 5 min read

How do I know if I am getting Osteoarthritis?
Not all joint pain is Osteoarthritis. There are many causes and best thing you can do if you are concerned about the source of joint pain is to see your local physiotherapist or GP. They can give you advice about what it might be and preventative strategies for osteoarthritis.
Will walking, moving or exercise make my osteoarthritis worse?


No! Movement and exercise are very much encouraged with osteoarthritis. Moving the affected joint helps move healthy fluid around the inside of the joint. This helps with reducing pain and increasing function (figure 1). Movement like walking also strengthens the muscles around the joint, which helps take the load off the joint and protect it. IMPORTANT TIP - we need the right amount of movement/exercise for it to be helpful. If the joint is used to the point that it becomes very sore, the inflammation that occurs is not optimal for the joint. Overworking to the point that it needs an extended period of rest means that there is overall less exercise. This is called the boom-bust cycle (figure 2)
I have tried exercising in the past, and it has not worked. What do I do?
There are lots of reasons why exercise might not have been effective for you. Some common things that can cause this are:
Incorrect amount of exercise - doing too much or too little exercise to cause meaningful change
The type of exercise - there can be different contributing factors to osteoarthritis, it is important that the correct one is prioritised to get the most out of exercise; if the wrong focus is chosen, exercise may not be effective
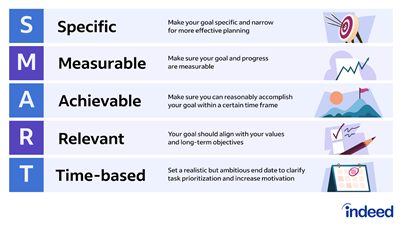
Unclear goal setting - If there are no clear, achievable goals set (see the next dot point on how to do this), it is really challenging to work towards/hit goals (or even to know if you have hit goals)
The period doing the exercises - Helping symptoms is a gradual, progressive process. While great changes can be felt early, often the longer the exercises are completed, the better the symptoms get. These things can take time. A good starting point is 6 weeks to see results; however, your physiotherapist may adjust this person-to-person.
Not progressing exercises - as you get better at completing your exercises, it's important that your exercises progress to match your new skills. This is important for seeing continual progress. Your progressions should be personalised and appropriate for you.
Infrequently completing exercise - Completing the exercises within your tolerance frequently is important for making progress
Not tracking outcomes - Sometimes you actually are making progress, for example, being able to walk further, but you may not even notice! It’s important to track what you are about to do now and monitor this as you complete your exercise. You may surprise yourself!
Physiotherapists are trained and specialise in creating and monitoring exercise in a way that addresses these factors. Talk with your physiotherapist about these areas and strategies/plans to make sure you are getting the most out of your exercise.
I sometimes forget my exercises and/or struggle to meet my goals. How can I stick to a good goal?Good, clear goals are critical for making progress and sticking to your plan. A tip for making goals is to use the SMART acronym. A goal that you can stick to is Specific, Measurable, Achievable, Relevant and Time-Based. An example is “I will increase my walking distance from 400m to 600m before knee pain starts in 3 weeks” (this goal is achievable for this person). Your physio can help you make SMART goals around your individual goals.
Can I change anything in my diet to help my osteoarthritis?
Diet and weight management definitely play a role in managing osteoarthritis. Decreasing overall weight reduces the amount of force through the joint, which plays a big role in decreasing symptoms. Good diet control and weight loss also reduce inflammation in the body. With many of the symptoms being felt because of inflammation, controlling this can help reduce pain and increase function. If support is needed for this, you can contact a local dietitian for more information.
Are there any creams or supportive braces that can help with my osteoarthritis?
Some people find creams (like fisiocrem, Voltaren or Deep Heat) or knee braces helpful for their pain, and this is great! It’s important to remember that while these remedies typically don’t cause harm, they don’t change your osteoarthritis or provide long-term relief, so they should ideally be used in combination with active strategies.
If one (or both) of my parents gets Osteoarthritis, will I eventually get it?
While there is a genetic link to osteoarthritis, it is not guaranteed that it will be passed down. It's important to remember that with preventative or management strategies, the osteoarthritis EXPERIENCE can be much different. Being proactive/active with treatment can make a big difference in reducing symptoms
Is there anything I can do to prevent getting Osteoarthritis?
Yes, there’s a lot you can do to help lower your risk. While there's no guaranteed way to prevent osteoarthritis completely, taking care of your joints and overall health can make a big difference.
One of the best things you can do is maintain a healthy weight and eat a balanced, nutritious diet. This reduces stress on your joints—especially your knees and hips.
If you've had a joint injury or surgery, it’s important to get proper rehabilitation. This helps restore strength and movement and prevents too much strain on the joint later on.
Staying active and strong, and using your joints is key—not just in prevention, but also in helping you manage things well if osteoarthritis ever does develop.
What's the difference between osteoarthritis and rheumatoid arthritis
While they sound the same, they are quite different conditions. Unlike osteoarthritis (which is a change in the cartilage around the joint), rheumatoid arthritis is an autoimmune disease. This means your immune system—the part of your body that fights illness—mistakenly attacks your own joints, thinking they’re harmful.
My friend has done the GLA:D program in the past. What is this, and should I consider it?
It is definitely something worth considering. The GLA:D program is a 6-week program made specifically for hip and knee osteoarthritis. It involves education sessions about what osteoarthritis is, its management, and exercises to help. All of this is facilitated by a trained physiotherapist. This program is now worldwide and has very strong evidence that it can be effective for reducing pain and other symptoms. There are criteria for joining this program, so to find out if you are eligible, speak with your Physiotherapist or GP.
Who do I contact if I think I have osteoarthritis?
If you are having joint pain and you are concerned it may be osteoarthritis, contact your local Physiotherapist and GP. They can help in diagnosis, treatment strategies and further referral if needed.
REMINDER – If you’d like to learn more, come to our free in-person education session – Understanding on Wednesday, August 13th at 6:30-7:30pm held at Good Country Physiotherapy (157 Smith St, Naracoorte).
Chloe Little and George D’Agostino
Fourth-year Physiotherapy Students at University of South Australia
Undertaking their Health Promotion placement at Good Country Physiotherapy, supervised by Angela Willsmore




Comments